Expectant mothers and their families facing high-risk or complicated pregnancies often need specialized care to guide them through their own unique challenges. A partnership between Community Hospital and The University of Chicago Medicine is bringing specialized Maternal-Fetal Medicine much closer to home making it more convenient for families.
Maternal-Fetal Medicine physicians partner with multiple caregivers to consult and co-manage complicated situations – chronic conditions including high blood pressure, diabetes or kidney disease – both before, during and after pregnancy. With this new collaboration, subspecialists from The University of Chicago Medicine supplement care already provided by Community Healthcare System’s team of obstetrician/gynecologists. These maternal-fetal specialists work in tandem with the expectant mother’s primary care physician to provide counseling, screening and fetal diagnostic testing.
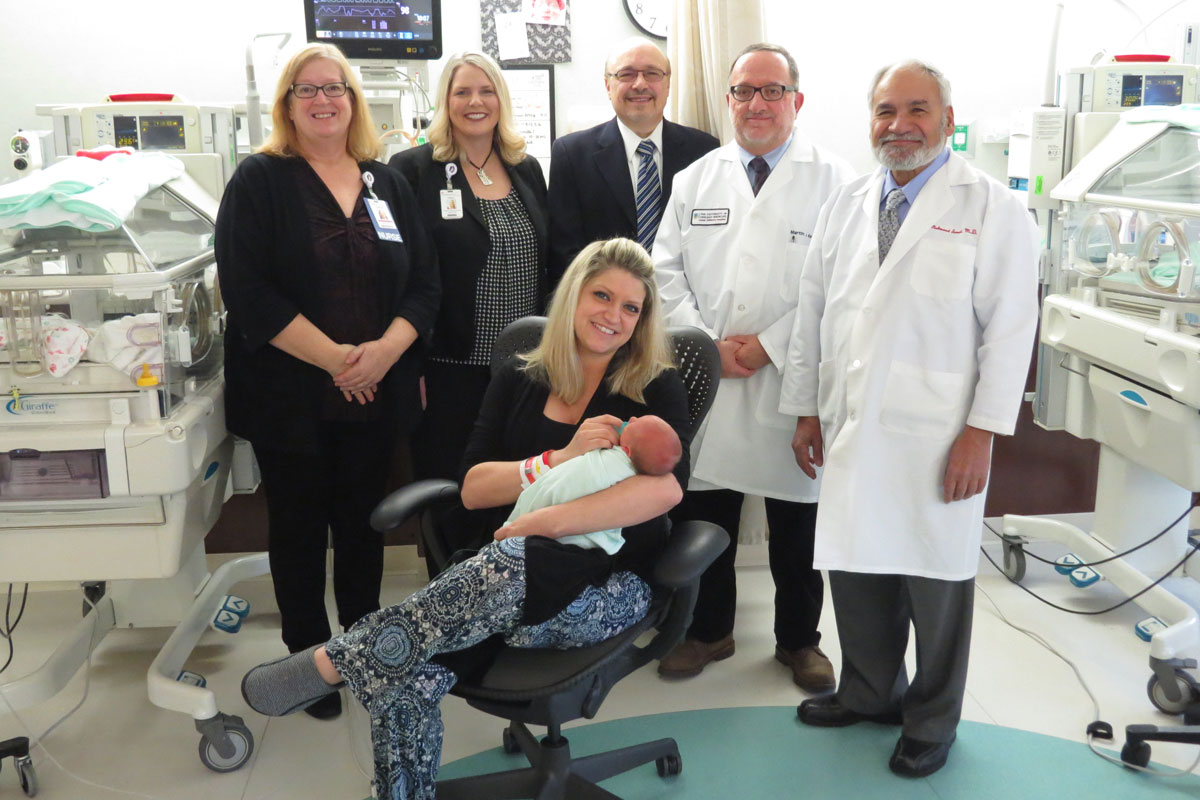
“Offering this level of expertise in managing high-risk situations means we have the knowledge and experience to guide women through every situation during this important time in her life,” said Carla Meyer, director of Patient Care Services. “Our team of maternal-fetal specialists, OB/GYNs, primary care physicians, nurses and other staff provide a woman and her family the critical support she needs to deliver a healthy baby.”
Previously, women with high-risk pregnancies living in Northwest Indiana would be referred to a hospital in a university setting to receive a more complex level of care.
“Some of the patients that may have been transferred before Maternal-Fetal Medicine was available locally now can stay closer to home and deliver in the community,” Meyer said. “It keeps the mom, the baby and the support system together. When the mom needs to deliver outside the community traveling back and forth puts stress on the family unit.”
“It is a win-win situation to have a group of subspecialists available to care for the mother,” explained Neonatologist Martin Kelly, MD, Clinical Associate, University of Chicago Medicine, Section of Neonatology and Community Healthcare Partner. “This means someone is always nearby to evaluate these patients whether it is through the inpatient setting at Community Hospital or at the University of Chicago’s outpatient clinic in Schererville. This ensures that the patient gets the best care possible closest to home. As far as patient care and convenience for families; it is much better and it helps that the rest of the care team is in close proximity.”
After identifying that there is a need, patients can be referred into the program by their OB/GYN. Expectant mothers with complications also can come directly to Community Hospital’s Emergency department for care. To enhance this source of inpatient care as of July, 2017, Community Hospital has made available “laborists” or specialized OB/GYNs round the clock to see patients with acute conditions that require consultation with a Maternal-Fetal Medicine physician.
“A number of patients, for example, have conditions that can be taken care of in their own community, but need consultation with a specialist to make sure the correct plan is being followed during pregnancy and to ensure that the baby is delivered safely in the Level III Neonatal Intensive Care Unit (NICU) at Community Hospital,” said Sarosh Rana, Associate Professor of Obstetrics & Gynecology Chief, Section of Maternal-Fetal Medicine, The University of Chicago Medicine. “Our partnership ensures that there is seamless continuity of care.”
In 2012, Community Hospital first partnered with The University of Chicago to make advanced care available 24 hours per day, seven days per week in the NICU. Community Hospital’s NICU is the only Northwest Indiana critical care facility to have in-house neonatologists round the clock. These neonatologists now serve as Community Healthcare Partners, working side-by-side with Community Healthcare System’s skilled team of neonatal nurses, respiratory, occupational, physical and speech therapists and audiologists to provide intensive intervention for infants with special medical needs.
All three hospitals of the Community Healthcare System, including Community Hospital sister hospitals St. Mary Medical Center in Hobart and St. Catherine Hospital in East Chicago, work in partnership with one another and The University of Chicago to provide a complete spectrum of medical services necessary for mothers and newborns. As part of that care, the neonatal transport system was set in place to establish a means to transfer critically-ill or premature newborns between hospitals.
“We had already worked with The University of Chicago for our neonatal care and our outpatient Maternal-Fetal Medicine program,” said Meyer. “Expanding to offer inpatient Maternal-Fetal Medicine consults was a natural progression of the partnership based on a growing need. This helps to provide continuum of care.”
Learn more about the services offered to support families during the birthing experience at Community Hospital. Visit comhs.org/services/family-birthing-centers.